Conditions
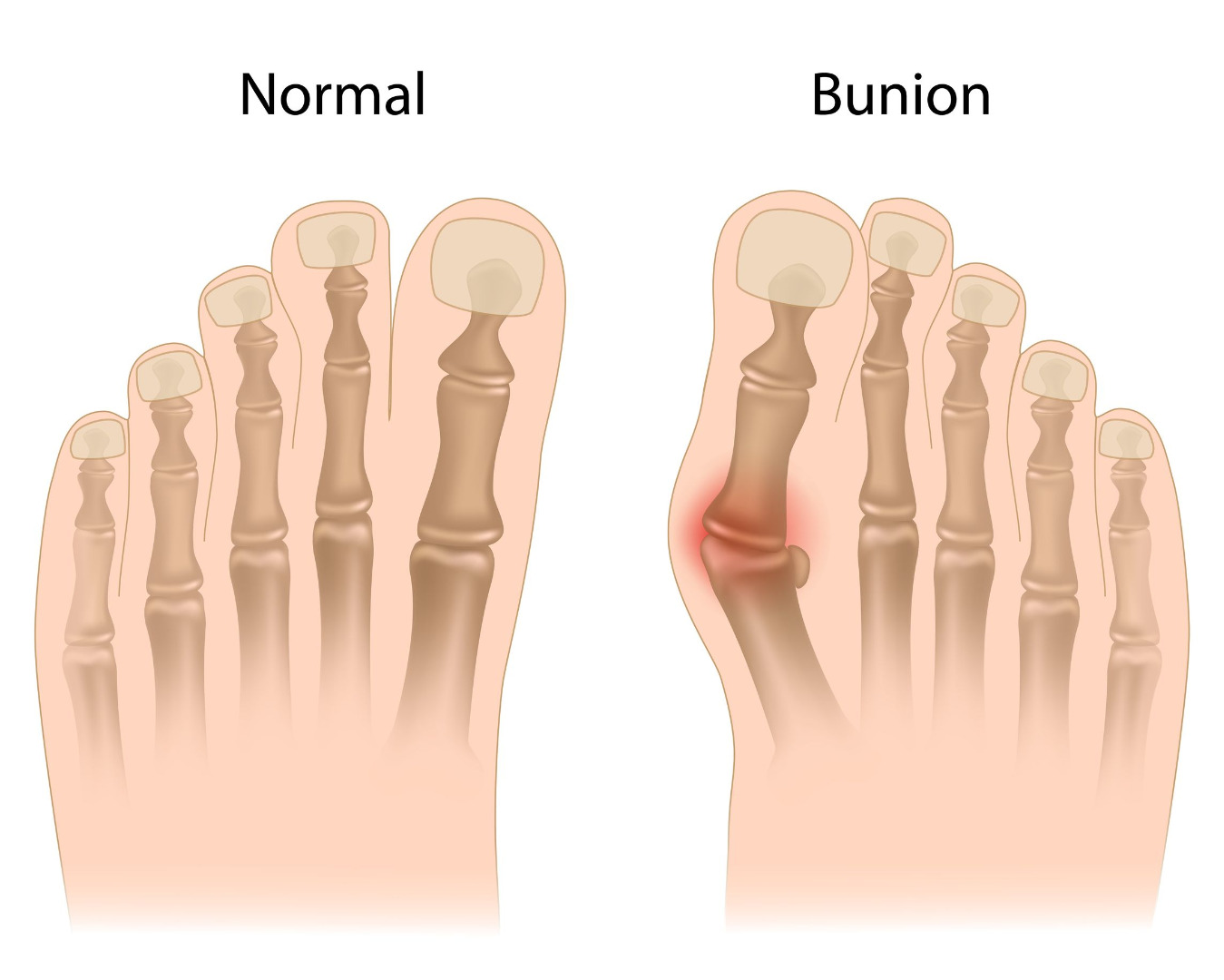
Bunions
Bunions often lead to discomfort over the prominence, especially during shoe wear. They at times run in family and are known to gradually worsen. The vast majority of bunions can be managed with non-operative treatment. Surgery is reserved for patients with persistent symptoms.
Patients with bunions will often describe pain over the prominent bump. They may also experience pain under the ball of the foot aggravated by standing and walking. Symptoms are often exacerbated by restrictive shoe wear, particularly shoes with a narrow toe box.
Over time, arthritis can also develop in the joint. With increased deformity or arthritic stiffness the big toe joint cannot be fully straightened to a normal position. The second toe carries more weight, and this can be an additional source of pain called metatarsalgia.
Persistent bunion pain that does not improve with shoe modification and other non-operative measures and those involving the second toe, altering its alignment or causing additional pain may require surgical correction.
When you come to see me, I will obtain weight-bearing x-rays of your foot after going through details of your symptoms. These x-rays would help us to decide the best treatment for your bunions. The initial treatment will be non-operative in form of properly fitted shoes, bunion pads, a toe spacer, bunion splints and soft shoe inserts. If you have already tried non operative treatments and your x-rays show severe deformity with arthritis, we would discuss operative treatment.
Surgery should only be considered for bunions that are moderately to severely painful. The type of operation that I would recommend would be dictated by the severity of your bunion deformity and associated arthritic changes in your joint.
Most surgical corrections would include:
-
Removal of the prominence on the inside of the foot (medial eminence).
-
Osteotomy to realign your bones to prevent the bunions recurrence
-
Removal of bony spurs or fusion of joints if severe arthritis and mal-alignment
-
Joint replacement
All bunion operations would be done as day case procedures so that you could return home on the same day. My team would make sure that you have nerve injections in your foot so as to minimise pain after your operation. You will be provided with a special shoe to walk on your heel and have physiotherapy after discharge. Your wound would be closed with dissolvable stitches. I would see you at 2 weeks for wound check and again at 6 weeks for a check x-ray. At this stage, you should be able to walk fully without any discomfort and should be able to use your own shoes. Most times you should be able to drive at 9 weeks and return to your recreational activities by three to six months.
Read More
Read Less
Ankle Sprain and Ligament Injuries
A sprained ankle is a very common injury. Ankle sprains usually occur as a result of an inversion injury where the foot turns inwards. It can result into injury to the ankle ligaments. These ligaments hold your ankle joint in position and protect it from abnormal movements such as twisting, turning, and rolling of the foot. During the sprains, these ligaments are stretched but if stretched more than they can handle, they can tear and result in your ankle joint giving way. If stretching continues, the joint surfaces can get damaged and may result into cartilage damage inside the ankle joint.
The three most commonly injured ligaments are:
A) On the outside of the ankle: ATFL (anterior talo-fibular ligament) and the CFL (calcaneofibular ligament).
B) On the inside of the ankle: Deltoid ligament.
C) Just above your ankle joint securing the ankle bones together : Syndesmosis

Symptoms
Sprained ankles present with pain and swelling but can have severe bruising, so that you think you may have broken it. In most cases you will be able to weight bear, and if you cannot then this usually indicates a more serious injury.
The majority of simple sprains recover fully within a few days without more treatment than RICE – Rest, Ice, Compression and Elevation. Early functional rehabilitation with the help of a physiotherapist can help maintain the flexibility, strength, co-ordination (proprioception) and stability of the ankle.
What happens if my ankle doesn’t settle?
A proportion of ankle sprains fail to settle and continue to cause pain, stiffness or giving way (instability). Those sprains that are not settling by 3 months, despite proper rehabilitation are called ‘chronic ankle sprains’
Chronic ankle sprains will need further investigation, to exclude scar tissue, localized damage to the joint surface or laxity of the ligaments that might respond to surgical treatment. Injury to joint surface or excessive scar tissue may benefit from an arthroscopy. If the ankle continues to give way, even after intensive physiotherapy, it might be necessary to repair or reconstruct the ligaments.
When you see me with ligament sprain that fails to settle, I would arrange for an MRI (magnetic resonance imaging) scan after careful examination to rule out injuries to your ligaments and ankle cartilage. Depending on the duration of your symptoms, I may arrange individualised physiotherapy sessions with my dedicated physio team or may advise operation to stabilise your ligaments.
If you require an operation to stabilise your joint, you will be in a leg cast for first 2 weeks. From two to six weeks, you would be in a special boot which would allow you ankle motion under the guided supervision of my physiotherapy team. You will be able to fully weight bear at 6 weeks and return to Sports by three months. If you have associated damage to the inside of your ankle joint, the rehabilitation may be longer.
Read More
Read Less
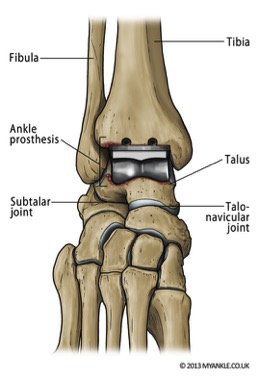
Ankle Replacement
Ankle replacement is a recognised alternative treatment to ankle fusion for Ankle arthritis. It remains an emerging technology and should only be performed by an expert who carries out sufficient numbers of ankle replacements each year.
Most ankle replacements have a mobile component, made of ultrahigh molecular weight polyethylene (hard wearing plastic), which sits freely between the two metal components and moves forwards and backwards slightly during ankle.
An ankle replacement is performed through an incision over the front of the ankle. The surgery takes between one and two hours. When you wake from surgery you will have a below knee partial cast, which may later be changed into a full cast at discharge. You may have to wear a cast for a period of up to 6 weeks. In some circumstances your surgeon may choose not to use a cast but may use a walker boot instead. You are likely to need crutches or a frame to help you walk. Depending on your situation, your surgeon may allow you to fully weight bear in cast once the wound has healed.
During your first appointment, I would arrange for an MRI or CT scan after careful history and examination to establish the diagnosis. I would discuss the treatment options based on your individual needs and scan findings. If you require Ankle replacement, I would go through the details of your surgery including benefits, risks and post operative rehabilitation. I use implants with proven benefits and long term survival rate. During your operation you will have nerve blocks to reduce post operative pain. Your first outpatient appointment after surgery will usually be at two weeks for wound check. You will also be given an appointment to see me in the out patients clinic at 6 – 8 weeks following your surgery. My physiotherapy team would work with you to regain functional range of movements following cast removal.
Read More
Read Less
Ankle Arthroscopy
An ankle arthroscopy is a key hole surgery that can be used to treat various injuries and disorders of the ankle. It typically involves two small incisions in the front of the ankle. A camera is placed in the joint through one incision which enables the surgeon to look inside the ankle joint. Through the second incision small instruments can be placed which help the surgeons to perform the procedure.
Ankle scope is used to address many different problems of the ankle. This typically includes synovitis (inflammation inside the joint), impingement due to presence of bony spurs, removal of loose bodies, ankle arthritis and osteochondral lesions (detached small cartilage inside the joint)
The procedure usually is performed as a day case. Recovery after this procedure typically is quick apart from ankle fusion. Most patients will be allowed to walk immediately once the wounds have healed.. In other cases a soft cast will be applied and the patient will stay off the leg for a period of time. This can typically range from 1-6 weeks.
The complication risks from ankle arthroscopy are very low about 3.5%, but can include: Infection, nerve and vessel injury, Deep Vein Thrombosis (Blood Clot), complex regional pain syndrome and Failure to resolve all symptoms
Read More
Read Less
Heel Pain, Achilles Tendinopathy and Plantar Fasciitis
Achilles Tendinopathy
Tendinopathy describes an unhappy Achilles tendon. Heel pain, plantar fasciitis and Achilles tendinopathy usually imply high tension within the unit. In the early phases of disease there may be inflammation of the lining around the tendon.
After a while the tendon is no longer inflamed but starts to degenerate which leads to micro tears, not visible from outside. Body attempts to repair this which then often results in a swollen bump on the heel or within the tendon.
With age, tendons become less stretchy (or less elastic) and also the blood supply to the mid-portion of the Achilles tendon reduces, and this means that in the mid 30’s to mid 40’s, Achilles tendon problems become more common.
The main symptoms are pain on the sole of the heel or around the Achilles tendon. Most times this is a burning ache, but sometimes could be a stabbing pain. You may feel a bump in your Achilles tendon and this is usually about 3-5cm above the heel bone and this represents a swollen tendon (non insertional). In insertional Achilles tendinopathy you may have a ‘pump bump’ which is where the swelling is close to where the tendon inserts into the bone and may represent a swollen fluid filled sac, called a bursa.

When you come to see me with Heel pain, I would build my diagnosis based on the history and findings of a clinical examination. It is not always necessary to perform further investigations but an ultra-sound scan or an MRI scan, can be helpful in certain cases.
The vast majority of patients with Achilles tendinopathy do not require surgery. The initial treatment normally is rest, ice, painkillers and physiotherapist guided stretching exercises. This can be very effective in trying to reduce the tension within these structures. Your physiotherapist will also assess your general posture and core stability and teach you specific exercises to help with this. Orthotics, injections and shock therapy are additional adjuncts that can be used before trying operative interventions.
Surgery
Surgery is only advised in those who have failed to improve with non-surgical treatments. This is because the results of surgery are unpredictable. We would proceed with surgery only after failed conservative management.
The surgical plan is to reduce the tension in the tendons, remove the degenerated tendon and reconstruct it if more than half of the tendon is excised in debridement. The surgery is done as a day case (unless you need to stay in for medical or social reasons). Your leg will be in a plaster for first 2 weeks to protect the tendon repair. After 2 weeks, you would be placed in a special boot which will allow you to put weight but will still protect the repair with wedges placed inside the shoes. The wedges are removed every week to improve the ankle movements. At 6 weeks, you will be out of boot and my physiotherapy team would work with you for guided Achilles tendon strengthening.
The surgery is successful to alleviate pain but can take time to regain function. There is 70 % success rate with debridement alone and around 80 % success rate with augmentation. With Haglund bony spur excision the success rate is 80 %. Most patients have much worse function prior to surgery and notice a significant improvement (usually by 6 months).
Read More
Read Less
Conditions
The implants I use have excellent results and low failure rates.
For all my procedures, my team will provide ‘ Regional Blocks ‘ to have a painless recovery from operation from day one.This helps in early mobilisation, shorter length of stay and accelerated rehabilitation. Most procedures I perform are suitable for day-case surgery (admitted, operated and discharged on the same day).
|